Invasive fungal sinusitis - symptoms, diagnosis, and treatment
- Dr. Koralla Raja Meghanadh

- Mar 27, 2022
- 5 min read
Updated: Apr 16, 2024
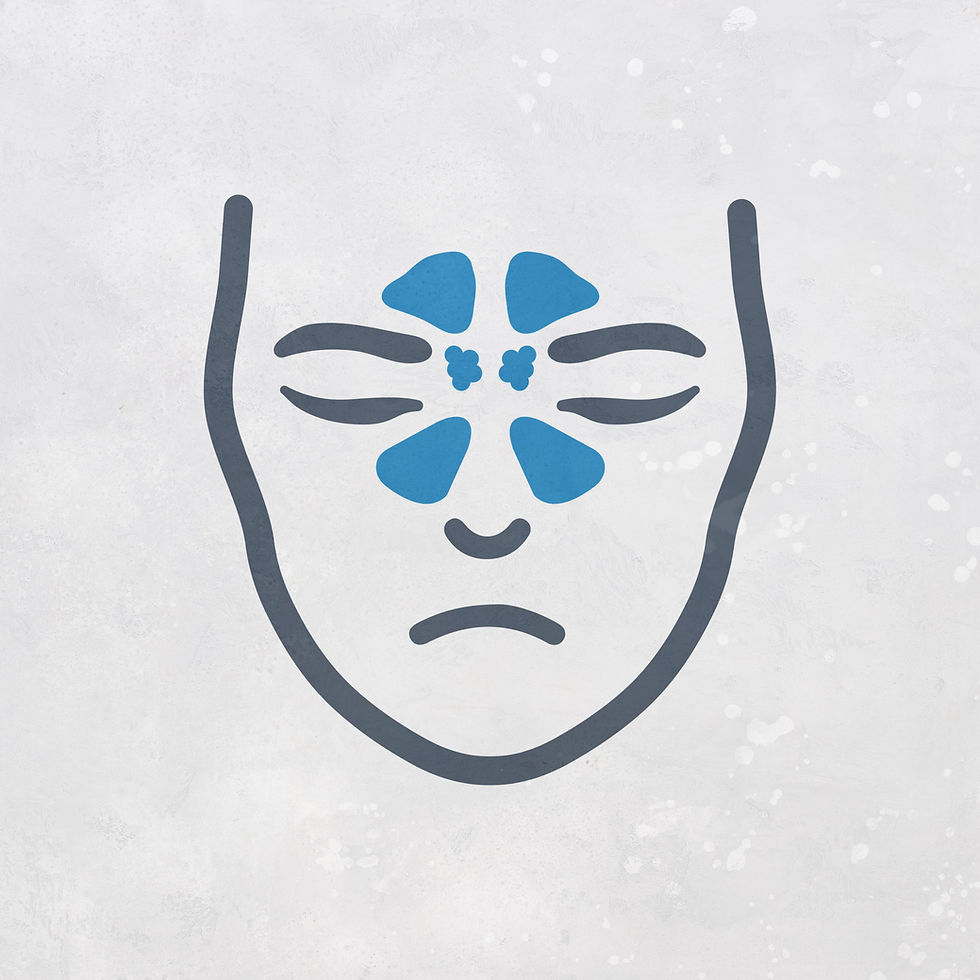
Invasive fungal sinusitis is a rare, severe condition where fungal infections spread from the sinuses to surrounding tissues. If not treated promptly, it can invade nearby structures like the eyes and brain, causing serious complications.
This article will explore the types of invasive fungal sinusitis, its symptoms, diagnostic methods, and treatment options to effectively manage the infection.

What is Invasive Fungal Sinusitis?
Invasive fungal sinusitis spreads beyond the sinuses into surrounding tissues, often due to a weakened immune system. While most fungal sinus infections are non-invasive, compromised immunity can turn them invasive, causing tissue damage.
Invasive fungal infections are more dangerous than non-invasive ones, though invasive cases don't require surgery, while non-invasive cases always do. A person may have both forms, requiring tailored treatment. In severe cases, the infection can spread to critical areas like the eyes or brain.
Types of Invasive Fungal Sinusitis
There are two types of invasive fungal sinusitis:
Granulomatous Invasive Fungal Sinusitis: Granulomas are well-developed immune system cells that surround the fungus and try to fight the infection. If these granulomas are present around the fungal infection, it will be granulomatous fungal sinusitis. Given the right combination of medicines, recovery is quicker for a granulomatous fungal sinus infection.
Non-granulomatous Invasive Fungal Sinusitis: In this form, granulomas are absent, making the infection more challenging to treat.
Invasive Fungal Sinusitis Symptoms
In invasive fungal sinusitis, infection can spread from the sinuses to other parts of nearby sinuses, causing symptoms like:
Pain and/or swelling in the eye, nose, teeth, or cheek
Vision disturbances – double vision or diminishing vision
Loosening of the teeth when the infection spreads to the jaw bone
Loss of sensation in the cheek
Swelling of the face if it spreads to the skin – a rare condition
When it spreads to the brain, the body part controlled by that part of a particular brain area will be affected.
Example: In one of the invasive fungal sinusitis cases seen by Dr. K. R. Meghanadh, the disease invaded the left side of the brain that controls the right arm, resulting in paralysis of the right arm.
Diagnosis of Invasive Fungal Sinusitis
Diagnosing invasive fungal sinusitis can be tricky and complicated, requiring a combination of techniques to ensure accuracy. It typically involves:
Biopsy: This procedure involves removing a small tissue sample for microscopic examination. Depending on the location, the biopsy may be performed under local or general anaesthesia.
Nasal Endoscopy, MRI, or CT Scans: The challenging aspect of the biopsy process is determining the most appropriate location for taking the sample. Tests like nasal endoscopy, MRI, and CT scans help determine the location.
Histopathology of Biopsy: Once a biopsy is obtained, the tissue undergoes histopathological analysis. Histopathology involves slicing a tissue sample into thin pieces and staining the cells' structures in these slices. These slices are observed under a microscope. Each disease will have specific signature characteristics when viewed under a microscope. If the fungus is in the tissue, it is an invasive infection. If it is invasive, the pathologist will look for granuloma formation. Moreover, pathologists may also use other staining methods to identify the characteristics and patterns of different cells to confirm the diagnosis.
The experience of the ENT specialist is crucial for an accurate diagnosis, as invasive and non-invasive infections can sometimes coexist in different sinuses and be left undiagnosed.
Invasive Fungal Sinusitis Treatment
The primary approach for treating invasive fungal sinusitis involves using oral antifungal medications. As the fungal is present in the tissues, the medication works effectively. Surgery, like removing infected tissue, is not needed.
Many doctors recommend extensive surgeries that involve removing parts of the nose, sinuses, and even parts of the face. However, Dr. K. R. Meghanadh suggests a less invasive approach. Based on his experience, he suggests that antifungal medications should be the main treatment rather than opting for surgeries that can lead to loss of function and disfigurement. Although the treatment might take years to complete, it is better not to opt for surgery in these cases.
Invasive Fungal Sinusitis Complication: Rare cases of infection spreading to the skin
In very rare cases, when the infection is ignored, misdiagnosed, or treated wrongly, the infection can spread from tissues to the facial skin. Here is a rare case seen by Dr. Meghanadh.
Rare extreme example case report by the author
A 23-year-old woman began experiencing swelling on her left cheek, which slowly worsened. She developed vision problems, a blocked nose, headaches, and noticeable facial disfigurement. Despite trying various treatments, including both allopathic and alternative medicine, for two years, her condition didn't improve. Eventually, she considered surgery with a plastic surgeon.

At age 25, just before she was going for plastic surgery she consulted the author, who suspected an invasive fungal granuloma. The diagnosis was confirmed, and treatment began with intravenous antifungal medications for 32 days, followed by oral medications. Her blood levels were monitored regularly.

Today, her facial appearance has improved significantly, and all her symptoms have resolved. With continued treatment, her face and skin are expected to return to normal within two years.
Takeaway from this case:
This case demonstrates that, even in advanced cases, antifungal treatment can effectively treat invasive fungal sinus infections without requiring surgery.
What Sets Invasive Fungal Sinusitis Apart from Other Types?
Here are three types of fungal sinusitis:
Non-invasive: The fungus stays confined to the sinus cavity.
Invasive: The fungus spreads into surrounding tissues.
Fulminant Invasive: A severe form where the fungus rapidly spreads into tissues and through blood vessels.
Invasive vs Non-invasive
Most fungal infections are non-invasive, but invasive fungal sinusitis can develop in people with weakened immunity. Non-invasive fungal sinusitis usually occurs in chronic sinusitis patients when the infection is left untreated for a long time. Though invasive infections are more dangerous, they can often be treated with antifungals. Non-invasive cases, however, require surgery since antifungals can't penetrate the sinuses. In some instances, both invasive and non-invasive infections can occur together.
Invasive vs. Fulminant Fungal Sinusitis
Although fulminant fungal infections are classified under invasive fungal sinusitis, the two are very different in practice. Invasive fungal sinusitis progresses slowly, taking years to reach nearby structures, while fulminant infections spread rapidly, often in weeks or days. If untreated, fulminant fungal sinusitis can be fatal within a couple of months.
Fulminant cases require not only oral antifungals but also powerful IV antifungals, often with intensive care monitoring. Extensive surgeries are needed to remove infected tissues. In contrast, invasive fungal sinusitis usually responds to oral antifungals and doesn't typically require surgery. Fulminant fungal infections are commonly called black fungus and white fungus infections.
An article by
FAQs
Can invasive fungal sinusitis be cured?
Yes, with the proper treatment, we can cure invasive fungal sinusitis. The primary approach for treating invasive fungal sinusitis involves using antifungal medications. Surgical intervention is not recommended, as the antifungal treatment is highly effective in managing the condition.


Comments